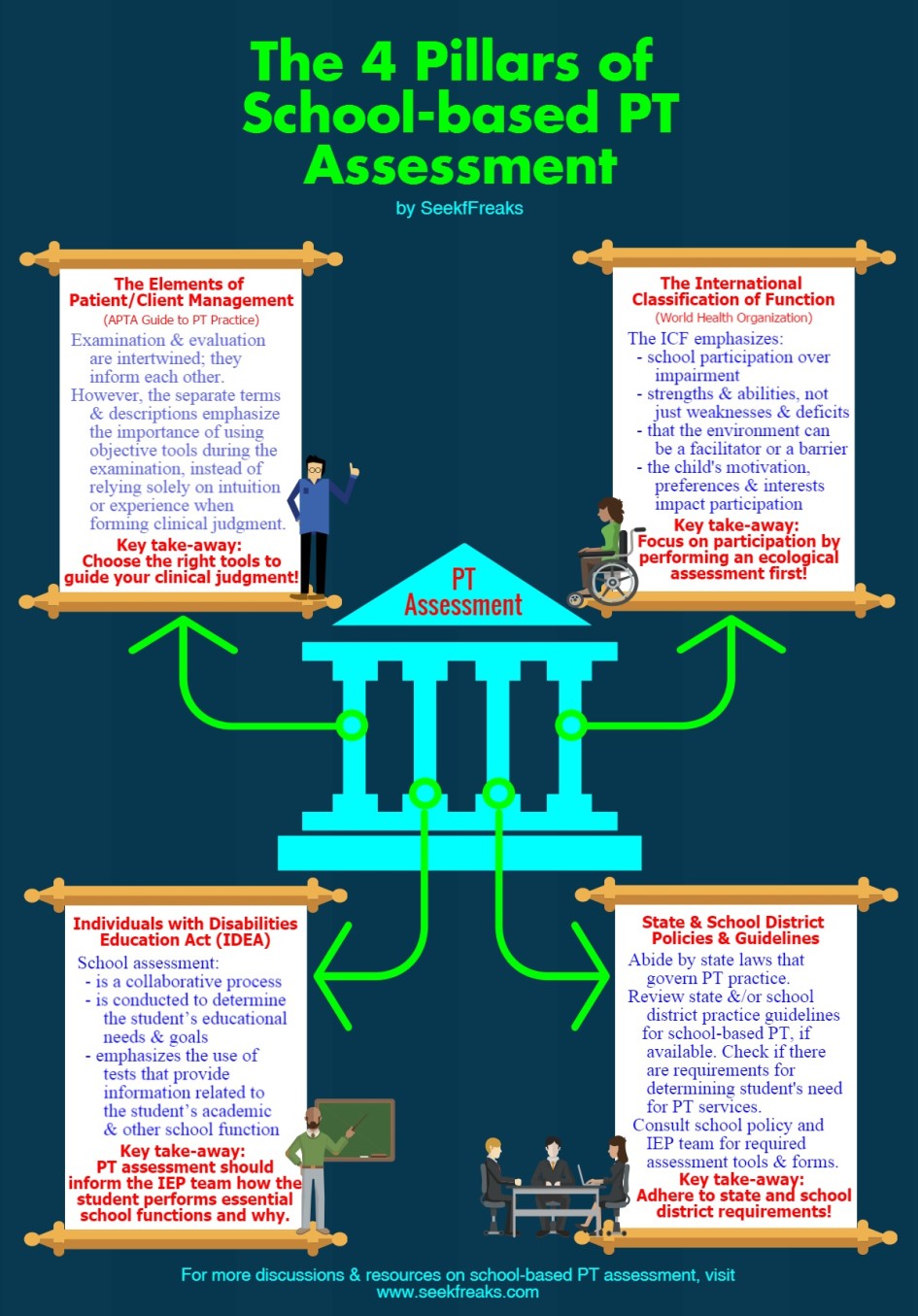
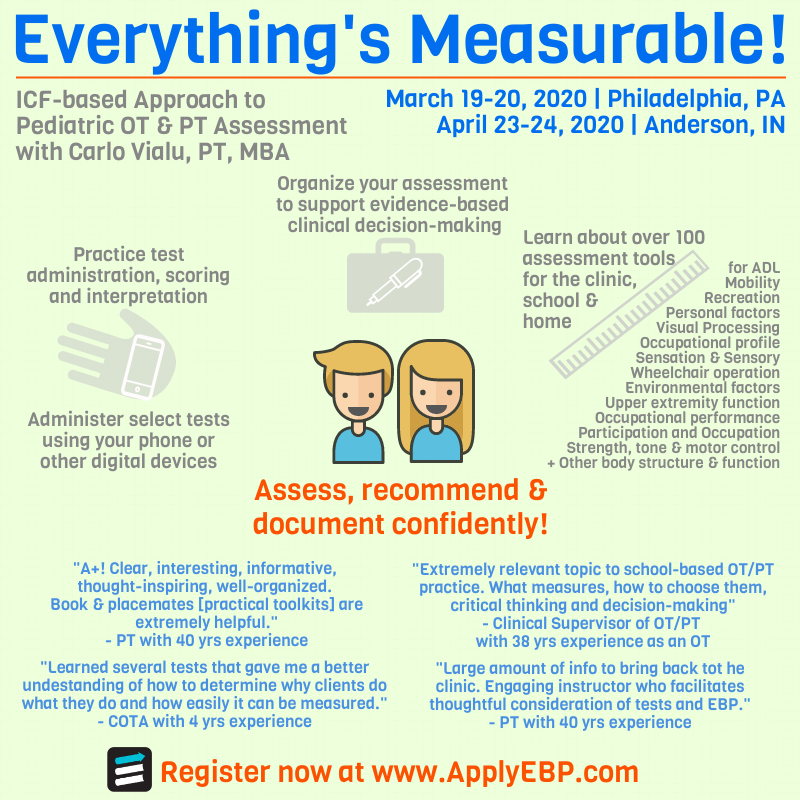
The author, Carlo Vialu, PT, MBA, is co-creator of SeekFreaks. He loves promoting function and participation for children and youth with disabilities, from our assessment to our interventions, via his continuing education courses: Train the Brain!, Everything’s Measurable! and The Well-Equipped Therapist! More about these courses after the article.

I still remember my first school-based PT assessment. Coming from an outpatient clinical setting, it was instinctive to utilize the best tests and measures in my toolkit to assess a student in a one-on-one setting. I quickly realized that school-based PT assessment is different! If the child is to succeed as a student with specific classroom and school expectations, it was clear that I had to adjust my framework for assessment.
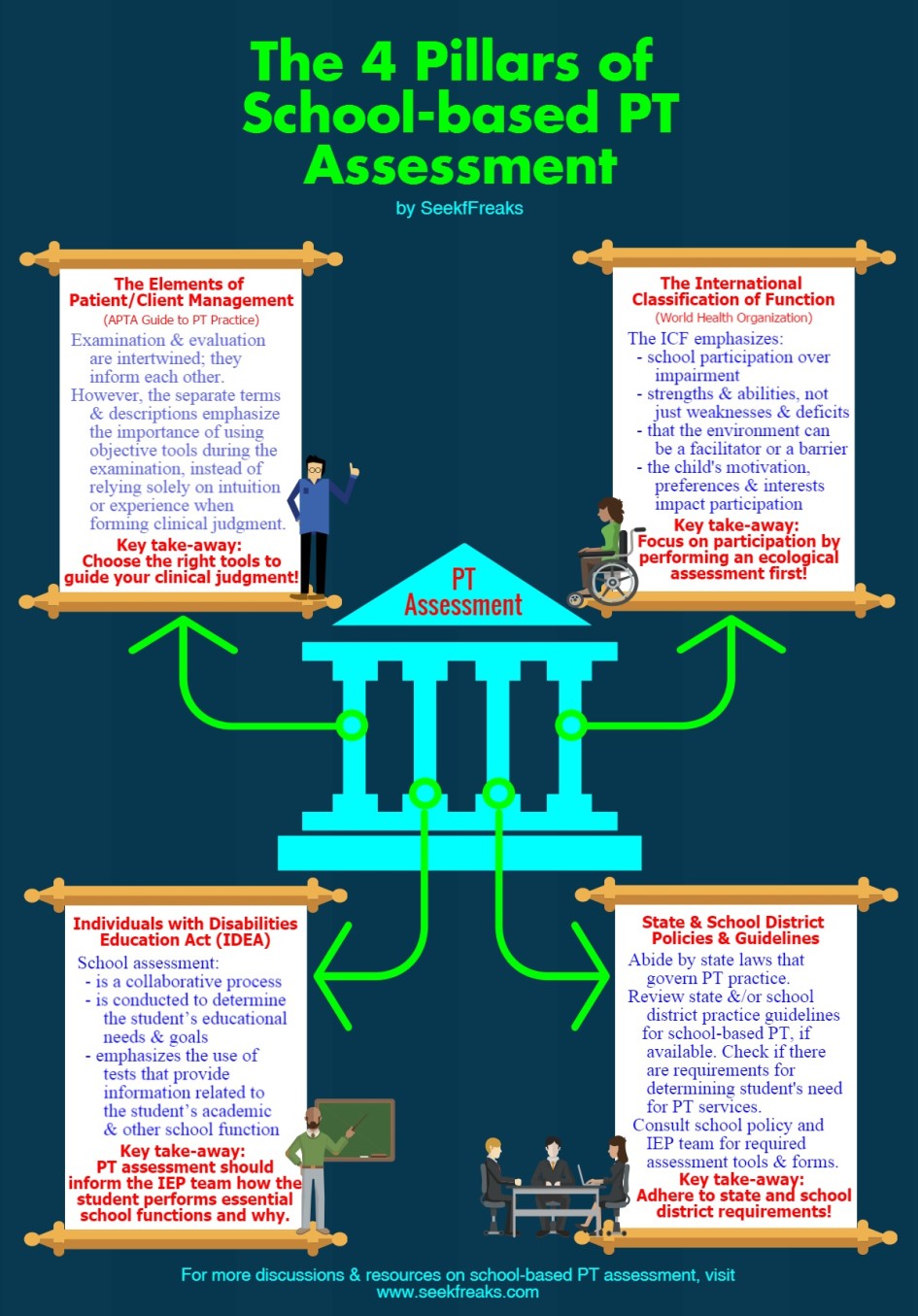
Today, we introduce you to the four pillars of school-based PT assessments. We hope this discussion will provide a solid foundational framework that will guide the way we conduct PT assessments and form clinical judgments. The 4 Pillars include:
We will discuss the 4 pillars in 4 easily-digestible articles, each covering one of the pillars.
Seek Freaks, FYI! APTA describes examination and evaluation as 2 distinct procedures (as will be discussed below), while IDEA does not differentiate evaluation from examination and simply uses the term evaluation. To avoid confusion in this article, we will use the term assessment to describe a process that includes both examination and evaluation.
1st Pillar: The Elements of Patient/Client Management
The APTA Guide to PT Practice describes 5 Elements of Patient/Client Management: Examination, Evaluation, Diagnosis, Prognosis and Intervention. Let’s look at the first two. The Guide defines examination as “the process of obtaining a history, performing a systems review, and selecting and administering tests and measures to gather data,” and evaluation as making “clinical judgments based on data gathered during the examination.”
While the delineation between the 2 seems to suggest 2 separate processes, in fact, they are intertwined, each informing the other. For example, the PT uses clinical judgment (evaluation) to select appropriate tests and measures (examination) that will help pinpoint the strengths, weaknesses and needs of the student.
The separate description, however, does emphasize the importance of using objective tools during the examination, instead of relying solely on intuition or experience when forming clinical judgment. A PT’s assumption may be that impaired balance and posture are causing the student’s difficulties moving within the classroom. This assumption must be tested by measures such as the Pediatric Balance Scale, Timed Up and Go, Timed Floor to Stand or others. Results from such tests may confirm or rule out the PT’s assumption. Either way, the therapist gets closer to the source of the child’s difficulty and the interventions that may be required to improve classroom performance and participation
Take-away: Choose the right tools to guide your clinical judgment.
Reference: American Physical Therapy Association. Guide to Physical Therapist Practice, 3.0 . Richmond, VA; 2014. http://guidetoptpractice.apta.org/.
2nd Pillar: The International Classification of Function
The World Health Organization’s introduction of the International Classification of Functioning, Disability, and Health (ICF) in 2001 was definitely an innovation. An innovation that shook the long-held belief (described below) espoused by the International Classification of Impairments, Disabilities and Handicap (ICIDH), it provided a new perspective to diseases and disabilities that resulted in new approaches to interventions. Let us look at the 2 models.
Figure 1. ICIDH
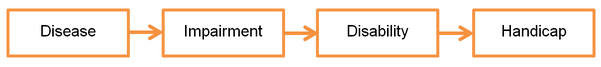
The ICIDH model is linear and deficit-based: a disease causes impairment (in body structure and function), that leads to a disability (in performing certain activities), that results in a handicap (or the inability to participate in societal functions). Unfortunately, this model also implies that to enhance a person’s participation in society, we must first cure the disease, fix the impairment and remove the disability. We know this is incorrect!
Figure 2. ICF
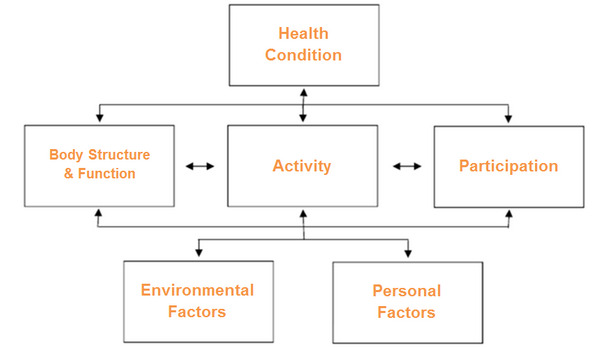
The ICF model, on the other hand, demonstrates multiple pathways of influence. Cause-and-effect is multi-directional, not linear. For example, while ICIDH implies that impairments in body structure and function influences participation, the ICF illustrates that participation can also influence body structure and function. In practice, this means that you do not have to focus on improving endurance (a component of body structure and function) prior to encouraging the student to participate in an aerobic physical education activity; rather, the student can participate in aerobic physical education activities to improve his endurance.
The ICF was also noteworthy for its focus on abilities, not deficits. In terms of assessments, we are charged to identify strengths, and not just weaknesses. This challenges us to see student with disabilities as students with abilities!
Moreover, the ICF includes the dynamic influences of environmental and personal factors on function. This inclusion highlights the fact that environmental and personal barriers can limit a student’s school performance and participation in the same way that the student’s health condition can. Addressing these barriers allows the student to perform and participate as expected in class, albeit in a modified manner, without necessarily correcting their impairments and disabilities.
How does the ICF framework affect PT assessment? The primary occupation of the child in the school is being a student. Therefore, the PT assessment must focus primarily on the student’s ability to participate despite his/her health condition, impairment or activity limitation. Additionally, the PT must also assess how the student’s environment (physical barriers, school routines, curricular and extracurricular demands) and personal factors (motivation, interests, preferences) impact his/her ability to participate.
In light of this, PTs must start their evaluation with an ecological assessment, which is essentially an observation of the student’s participation in class routine and activities throughout the school environment. It provides insight on how the student performs in comparison with his peers, whether the student is meeting class expectations, and how the demands of the physical environment and school tasks are influencing the student’s ability to participate. Participation restrictions identified through this ecological assessment would then warrant a closer examination of the student’s body structure and function. As discussed in the 1st Pillar of School-Based PT Assessment, the PT should use multiple appropriate tests and measures to identify the factors contributing to the participation restriction, and determine whether PT is the best school-based service to address such restriction.
You can learn more about the ICF with the SeekFreaks’ article Recognizing ICF Domain Words…Amusing Musings.
Take-away: Focus on participation by performing an ecological assessment first!
Reference: Simeonsson R, Leonardi M, Lollar D, Bjorck-Akesson E, Hollenweger J, Martinuzzi A. Applying the International Classification of Functioning, Disability and Health (ICF) to measure childhood disability. Disabil Rehabil. 2003;25(11):602-610.
3rd Pillar: Individuals with Disabilities Education Act (IDEA)
The requirements of IDEA differentiate a PT assessment in a school setting compared to other practice settings. Sec. 300.304 of IDEA describes the requirements for assessment procedures (click here for a complete list). Let’s discuss some of its contents.
School assessment is a collaborative process. The PT assessment is one of many assessments that are conducted to determine the student’s educational needs. In an outpatient setting, a PT assessment can by itself be used to decide the client’s intervention plan. In an educational setting, the PT assessment’s main purpose is to provide the IEP team information regarding student’s performance. The team uses this information to determine the student’s eligibility for special education services and the content of the student’s Individualized Education Program. All decisions, including the need for PT services, are decided via consensus. This does not mean that the PT’s voice is less than those of others, but rather that the team must prioritize the needs and goals of the student for this IEP period and decide the services that can best address those goals in the least restrictive manner.
Tools that Assist in Determining the Educational Needs of the Student
School assessment focuses on identifying the educational needs of the student. This reinforces the use of ecological assessment. It also emphasizes the importance of using tests and measures that provide information related to the student’s academic and other school function. The PT must describe how the student’s performance in those tests relate to the student’s difficulties in school.
Tools that Assess Factors that Influence Participation
Sec. 300.304.b.3 requires the use of “technically sound instruments that may assess the relative contribution of cognitive and behavioral factors, in addition to physical or developmental factors.” Thus, tests and measures should be chosen thoughtfully. They should include those that will help pinpoint the factors that contribute to the student’s difficulties in accessing and participating in their education. The determination of such factors can then help the IEP team in determining which services would make the biggest difference in addressing the student’s needs.
Take-away: Your assessment should inform the IEP team how the student performs and why.
4th Pillar: State and School District Regulations, Policies and Guidelines
First, let me point out the obvious, as PTs we are licensed by the state where we practice. Therefore, our practice is limited by what state law permits us to perform. To maintain the good standing of our license, we should ensure that we are following the regulations, not just when we are providing interventions, but also when we are conducting assessments. In particular, take note of requirements for working with minors (which is most of our caseload). It is highly likely that you need parent/guardian consent, but do you need a doctor’s note to assess a child?
Some state and school districts also have guidelines for school-based PT practice. You can use our Practice Guide Map to see if your state has one. If you do, you may find specific guidance when conducting an assessment and to see if there are eligibility requirements for PT services.
Florida, for example, uses the Considerations for Educationally Relevant Therapy (CERT) Form, while Oregon has an Eligibility Screening Tool. The Louisiana and South Dakota guidelines mention measures of developmental delay to qualify students for services, whereas New Jersey has a criteria that apply only to pre-schoolers.
Finally, each school district and each school has their own policies that need to be followed when conducting assessments. Consult the IEP team. Find the specific assessment tools and forms required. In school districts, where there are no required assessment forms, it will benefit you and your colleagues to create a uniform way of documenting an assessment. Incorporate what we have discussed in the past weeks, such as including an ecological assessment, and test and measure sections.
Take-away: Adhere to state and school district requirements!
The take-aways from the 4 Pillars we have covered should shape an efficient school-based PT assessment. PT assessment can become more meaningful by:
The physical therapist must also be aware that school assessment is a collaborative process: decisions are made not by any one individual but by the whole IEP team.
Freakishly Fast Poll
Seeking Your Views
Do you think the APTA’s Elements of Patient/Client Management is applicable to school-based practice? If not, how do you think it can be made applicable to school-based practice?
What is your least favorite test? Why?
Leave your answers and comments below.
Readers of this article also read these: